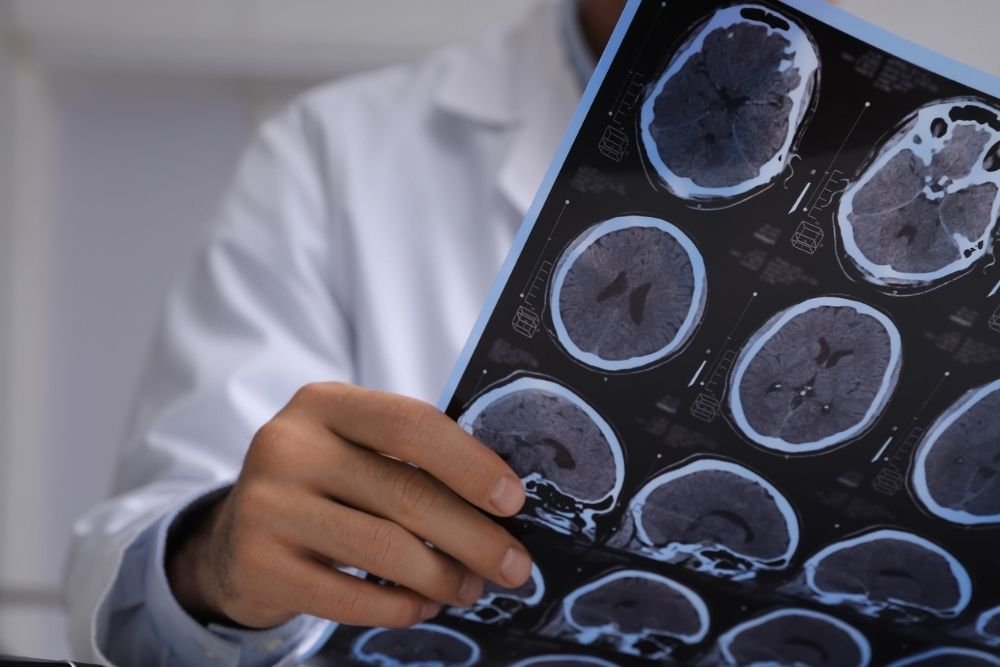
Substance use disorder (SUD) can show up in your habits, your reactions, and your roughest days, but your brain also carries a big part of your substance-use picture. If you’ve ever read our deep dive on the blacked-out brain and thought: yep, that sounds familiar, then you already know substances impact your brain’s ability to store memory. But neuroimages can show how substance use affects so much more of the brain than just memory.
Neuroimages from MRIs, MRSs, PET scans, and EEGs can act like snapshots of your brain during different moments. Here’s a rundown of the main types of neuroimages:
- MRI and fMRI. MRI captures clear pictures of your brain’s structure, and functional MRI shows which parts light up when you think, feel, or react.
- PET and SPECT. These scans follow tiny tracers that show how your brain uses energy and chemicals (like dopamine).
- EEG and MEG. These tools track electrical and magnetic signals that your brain sends out. They act fast and help researchers see how your brain responds in real time.
- MRS. This technique lets researchers look at brain chemistry when they’re studying mood issues or substance-related changes.
This skimmable neuroscience review can walk you through how this technology helps scientists study folks with substance issues and how to treat them with evidence-based methods. In fact, neuroimaging and other modern methods are part of the reason why you can step into residential treatment at Waypoint Recovery Center and receive scientifically-informed care that meets you exactly where you’re at.
Which Parts of the Brain SUD Impacts
As this scientific overview explains, repeated substance use can impact the brain’s reward circuits along with its planning and self-control circuits. That’s why you’re not imagining your brain arguing with you about cutting out substances.
Your reward system loves anything that feels good or comforting (food, connection, cozy blankets), and substances slide right into that same pathway. Over time, that pathway can encroach on everything around it, and that’s a huge part of why quitting substances can feel impossible.
Animal studies described in this imaging review also show that substance exposure itself can change brain circuits—so you’re not imagining the struggle. Your brain simply learns patterns, and with support, it can learn new ones.
But if we want to get into the nitty-gritty of SUD’s impact on the brain, we can look at the main areas that show up time and time again on scans:
- Striatum and nucleus accumbens. Neuroimaging studies show that these regions react strongly when people see substance-related cues. Stronger reactions often trigger higher cravings.
- Prefrontal cortex. This front-of-the-brain area helps you pause, think, and choose. This part can struggle when SUD is active, which helps explain why impulses sometimes win even when you know what you want long-term.
- Anterior cingulate cortex. This region helps you shift attention and manage inner conflict, and it may fire differently if you’re dealing with substance issues.
- Amygdala and stress circuits. Your amygdala handles stress and big feelings. One neuroimaging review on opioid recovery showed tightened amygdala connections with reward centers, which fits with the very real feeling that stress can send cravings through the roof.
What Neuroimages Tell Us About Recovery
Here’s the part most people find comforting: neuroimages don’t just show where the brain struggles. They can show healing, too. Neuroplasticity, how your brain stays capable of learning and rewiring, plays a huge role in that healing.
This study on neuroplasticity shows that your brain’s wiring can strengthen with practice, meaning repeating healthier patterns can literally help your brain kick SUD. That’s the heart of recovery. MRI research supports this idea too: both brain structure and function can change when you give it consistent, supportive experiences.
Recovery doesn’t happen overnight, but it absolutely happens. You practice new skills, you reach out instead of isolating, you build routines that support a substance-free life: that’s how neuroplasticity can benefit your recovery.
Find Recovery For Substance Use Disorder in South Carolina
Now you’ve seen how neuroimages work, what they show, and why they give real hope about your brain’s ability to heal. If you want a simple guide to what your recovery journey might look like, we break it down in this easy overview of the phases of recovery.
Whether you explore care in Cameron or North Charleston, you’ll enter our doors as a client who deserves understanding, patience, and a plan. Every small choice you make afterward can propel you toward a substance-free future.